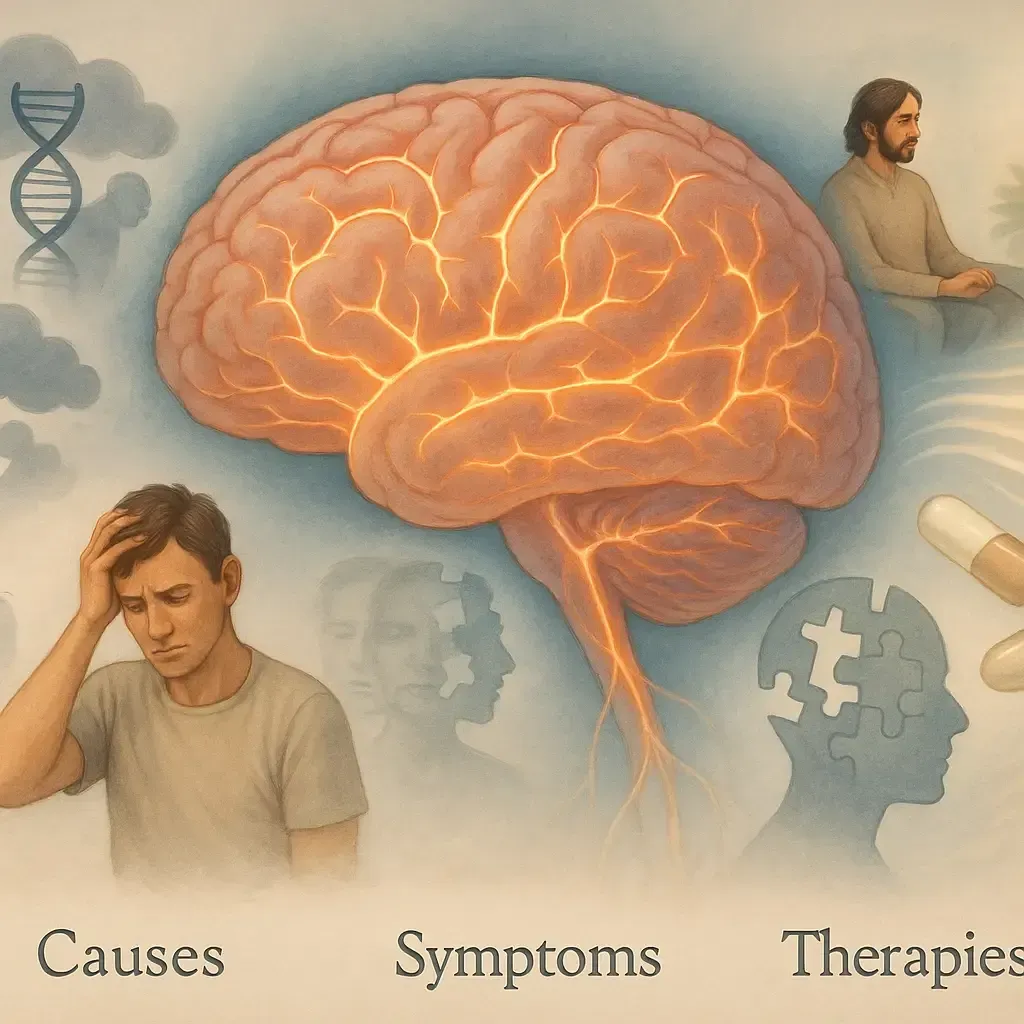
Understanding Cognitive Disorders: Causes, Symptoms, and Effective Therapies
Cognitive disorders affect how we think, remember, plan, communicate, and make decisions. Early evaluation matters: many causes are treatable or manageable, and the right therapy plan can protect independence and quality of life. This guide reviews causes, common symptoms, and proven therapies including cognitive behavioral therapy for general anxiety disorder (GAD), treatments for cognitive communication disorder, and how to find an Alzheimer’s and cognitive disorder specialist in Hagerstown, MD or a cognitive disorder specialist in Cumberland, MD.
At a glance (quick facts)
Cognitive disorders range from mild cognitive impairment (MCI) to dementias (e.g., Alzheimer’s), as well as vascular, Lewy body, frontotemporal, traumatic brain injury (TBI), and metabolic or medication‑related conditions.
Symptoms often include memory loss, slowed processing, word‑finding difficulty, attention and planning problems, mood changes, and communication challenges.
Effective care is multidisciplinary: neurology, neuropsychology, speech‑language pathology (for cognitive communication disorder), occupational therapy, and psychotherapy, such as CBT for GAD.
Lifestyle pillars sleep, exercise, blood pressure/sugar control, hearing/vision care, and social engagement help protect brain health at any stage.
What counts as a “cognitive disorder”?
“Cognitive disorder” is an umbrella term for conditions that disrupt mental processes. Common categories include:
Neurodegenerative: Alzheimer’s disease, Lewy body dementia, frontotemporal dementia.
Vascular: Strokes or chronic small‑vessel changes that impair attention, speed, and planning.
Traumatic: Concussion/TBI with persistent thinking and communication problems.
Medical/Metabolic: Thyroid issues, B12 deficiency, sleep apnea, infections, medication side effects, depression/anxiety.
Mild Cognitive Impairment (MCI): Measurable decline that does not yet impair basic daily activities. Some remain stable or improve with treatment and lifestyle change.
note on “cognitive processing disorder”
“Cognitive processing disorder” is not a formal diagnosis in DSM‑5, but people use the phrase to describe slowed processing speed or difficulty handling complex information after TBI, stroke, ADHD, mood disorders, or aging. Clinicians assess this with neuropsychological testing and target it with cognitive rehabilitation, compensatory strategies, and when appropriate medication or mood/anxiety treatment.
Cognitive communication disorder (and why SLPs are essential)
Cognitive communication disorder refers to communication problems caused by impaired cognition attention, memory, executive function, or social cognition. It often follows stroke, TBI, brain tumors, or neurodegenerative disease.
Common signs:
Trouble following conversations in noise or multitasking while talking
Disorganized storytelling, tangents, or missing key details
Word‑finding difficulty and slowed verbal responses
Reduced awareness of listener needs or social cues
Treatment: A speech‑language pathologist (SLP) provides metacognitive strategy training, memory aids (notebooks, apps, calendars), errorless learning, attention training, pragmatic/social communication work, and family education so communication stays effective at home and work.
Symptoms that deserve an evaluation
New memory lapses (repeating questions, missed appointments)
Slowed processing, trouble with bills, recipes, or technology
Language changes: word‑finding problems, mixing up names, halting speech
Spatial disorientation: getting lost in familiar places
Mood/behavior: apathy, irritability, anxiety, hallucinations (especially with visual hallucinations consider Lewy body)
Functional decline: errors at work, medication mistakes, falls


How specialists diagnose cognitive disorders
A thorough workup typically includes:
History & neuro exam (timeline, sleep, mood, medications, substance use).
Cognitive screening (e.g., MoCA/MMSE) and, when needed, formal neuropsychological testing for attention, memory, language, visuospatial, and executive functions.
Labs (B12, thyroid, infections, metabolic panels), sleep apnea screening, depression/anxiety assessment.
Brain imaging (MRI/CT) when indicated to evaluate strokes, tumors, or patterns consistent with Alzheimer’s or other neurodegenerative diseases.
Functional and safety assessment (driving, finances, fall risk).
Evidence‑based therapies
1)Treat the cause and optimize brain health
Correct reversible contributors (thyroid, B12, sleep apnea, medication side effects, hearing/vision deficits, uncontrolled diabetes or hypertension).
For Alzheimer’s disease and some dementias, clinicians may use cholinesterase inhibitors or memantine; for vascular cognitive impairment, aggressive vascular risk management (BP, lipids, glucose, exercise) is key.
Exercise (aerobic + strength 150 min/week), Mediterranean‑style diet, 7–8 hours sleep, smoking cessation, social and cognitive engagement all support cognition.
2) Cognitive rehabilitation & speech‑language therapy
Goal‑oriented training for attention, memory, and executive function
Compensatory tools: checklists, planners, smartphone reminders, voice assistants
Task modification: break steps into chunks; reduce distractions
Family coaching to create supportive communication environments
3) Psychotherapy: cognitive behavioral therapy for general anxiety disorder
Anxiety impairs focus and memory, and CBT is the first-line treatment for GAD.
Psychoeducation about worry cycles and the mind body link
Cognitive restructuring to challenge catastrophic thoughts
Worry exposure & scheduling (set “worry time,” postpone reassurance‑seeking)
Relaxation training (diaphragmatic breathing, progressive muscle relaxation)
CBT typically lasts 10–20 sessions, focusing on problem-solving, behavioral activation, and progress tracking with tools like GAD-7.
4) Caregiver support & planning
Caregiver training reduces burnout and hospitalizations.
Discuss advance directives, driving safety, fall prevention, and community resources early.

Cognitive Disorder & Memory Care Clinic in Hagerstown, MD
At our Hagerstown, MD clinic (11110 Medical Campus Rd #151, Hagerstown, MD 21742), we provide specialized care for memory loss, cognitive decline, anxiety-related issues, and recovery after stroke or TBI. Our services include dementia evaluations, MCI monitoring, Alzheimer’s care planning, medication management, and referrals for cognitive communication disorder therapy and CBT for anxiety or sleep concerns. Our Hagerstown team delivers compassionate, evidence-based care to support both patients and caregivers in their neurological and mental wellness journey.
Cognitive Evaluation & Therapy Services in Cumberland, MD
At our Cumberland, MD clinic (924 Seton Dr Suite C, Cumberland, MD 21502), we provide comprehensive cognitive testing, vascular risk management, speech-language therapy coordination, and care planning for complex conditions like Lewy body dementia or frontotemporal disorders. Our team uses thorough screening and neurologic evaluation to distinguish cognitive impairment from anxiety or mood-related causes, ensuring patients receive tailored, effective treatment. Many patients also ask, “Is Parkinson’s Disease a neuromuscular disorder?” While Parkinson’s is primarily a neurological disorder that affects movement, it shares overlapping symptoms with neuromuscular conditions, which makes accurate diagnosis and specialized care essential.
Get Expert Help

If you or a loved one is experiencing memory loss or cognitive decline, early diagnosis is key to effective management. Consult with our neurology specialists for personalized assessment and care plans.
Our Locations
Frequently Asked Questions
1. Is “cognitive processing disorder” the same as dementia?
No. It’s an informal term people use for processing‑speed or information‑handling problems. Dementia refers to persistent, progressive cognitive decline that impairs daily function. Processing‑speed issues can occur in many conditions—including anxiety—and may improve with treatment.
2. How is a cognitive communication disorder treated?
With speech‑language therapy focused on attention, memory, organization, social communication, and practical strategies (e.g., note systems, cueing, environmental modifications).
3. Does CBT really help thinking problems?
Indirectly, yes. CBT for generalized anxiety reduces excessive worry and physiological arousal, which frees up mental resources for memory and attention. It’s often part of a combined plan.
4. When should I see a specialist?
If memory loss, confusion, language problems, or personality changes persist for weeks, interfere with work/home life, or suddenly worsen, schedule a specialist visit. Sudden, severe symptoms warrant emergency care.
5. What can families do today?
List medications, bring a timeline of changes, track sleep and mood, organize legal documents, and begin daily routines that include exercise, social contact, and structured reminders.
To learn more about our experience or discuss your treatment options, please call us at (301) 797-7600 or schedule a consultation today!
Get our wellness newsletter
Filter out the noise and nurture your inbox with health and wellness advice that’s inclusive and rooted in medical expertise.
Contact Us
Complaint and Queries
(301) 517-7636
About | Careers
© Copyright 2026. Mir Neurology. All Rights Reserved.
A Part of Highland Healthy Living. Powered By CareSyncMarketing